

In addition, neurotoxicity is reported to be associated with the increasing cumulative dose of the paclitaxel. In particular, during the weekly administered paclitaxel regimen, patients are found feeling uncomfortable due to arthralgia and myalgia, taste changes, peripheral neuropathy, fatigue, cognitive problems, and insomnia.
#Taxol taxic levels in thebrain skin
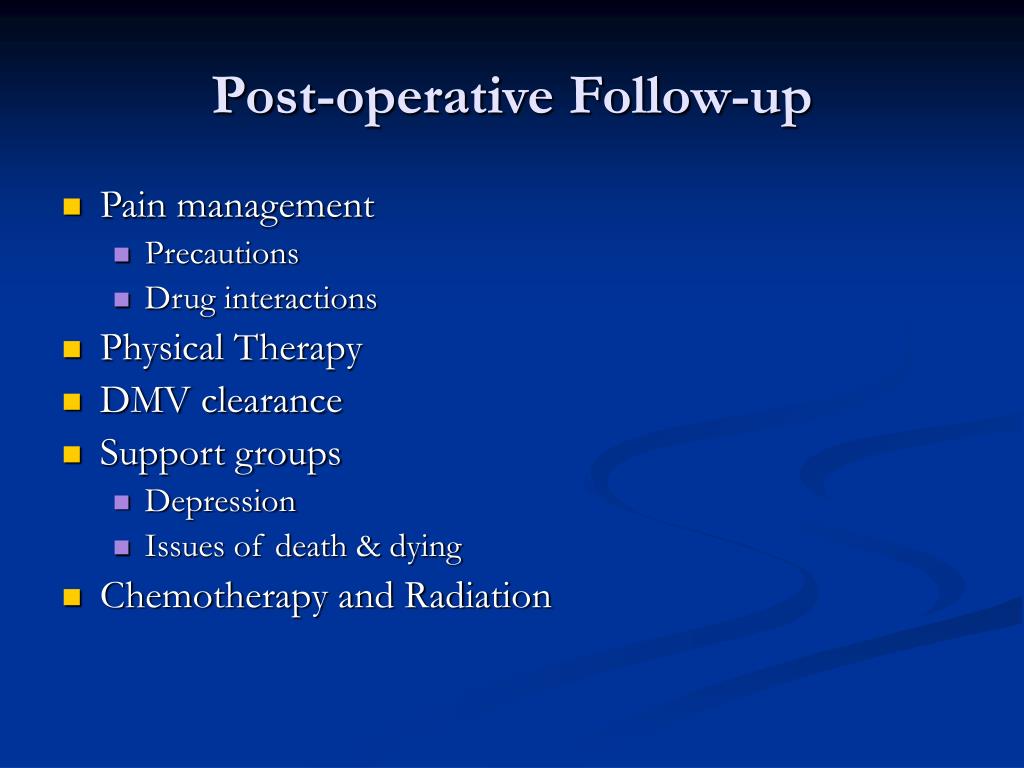
Paclitaxel often causes significant symptoms such as neutropenia, nausea, vomiting, diarrhea, oral mucositis, amenorrhea, alopecia, arthralgia, myalgia, peripheral neuropathy, skin and nail changes, liver and renal toxicity, and hypersensitivity reactions in BC patients depending on the number of cycles, and the dose administered. In particular, neurons are frequently affected by paclitaxel even though they are not dividing cells. Paclitaxel stabilizes the microtubule by binding to the lumens of the cell, stops mitosis, and eventually causes apoptosis. Dynamic instability of microtubules in the cell is necessary for mitosis. Paclitaxel, which cannot cross the blood–brain barrier, induces symptoms by causing toxic effects in the periphery. With the increasing clinical use of paclitaxel in BC, it is reported that therapeutic response, survival, and disease-free survival rates have increased. Paclitaxel is a taxane group drug and can be administered weekly (12 weeks) or every 21 days (four cycles) after four cycles of Adriamycin–cyclophosphamide (AC) treatment in patients with early-stage BC. Paclitaxel is frequently preferred during adjuvant and neoadjuvant therapies. In recent years, adjuvant and neoadjuvant systemic therapies have started to take an important place in BC treatment to reduce the associated mortality rate, in addition to the classical treatment methods such as surgery, chemotherapy, and radiotherapy. In addition, since the risk of depression increases over time in patients receiving paclitaxel, nurses should periodically screen the risk of depression, and timely consult the patients for the appropriate support.īreast cancer (BC) is the most common type of cancer among women worldwide, causing significant rates of mortality and morbidity. Better management of the symptoms that increase with the paclitaxel regimen with repeated interviews under the supervision of the nurse will also prevent the deterioration of body perception. The oncology nurse should comprehensively evaluate the patients who scheduled to receive paclitaxel treatment, and provide counseling to the patients during these specific weeks. The mean scores of the anxiety subscale of the HADS scale decreased at the T 3, T 4, and T 5 compared to T 1 ( F = 6.865, p < 0.001), and the mean scores of the depression subscale significantly increased at the T 5 compared to T 1 ( F = 3.708, p = 0.006). The mean scores of BPS significantly decreased at T 2, T 4, and T 5 compared to T 1 ( F = 8.152, p < 0.001). The frequency of needling and numbness in hands and feet, pain, and skin or nail changes significantly increased in the subsequent assessment points (T 2, T 3, T 4, and T 5) compared to the initial assessment (T 1) ( p < 0.05). Data was analyzed using descriptive statistics, Cochrane Q, and linear mix model regression analysis. “Chemotherapy Symptom Assessment Scale (C-SAS),” “Body Perception Scale (BPS),” and “Hospital Anxiety and Depression Scale (HADS)” were applied at five time points (T 1, before the first Paclitaxel infusion T 2, at the end of first cycle T 3, at the end of fourth cycle T 4, at the end of eighth cycle T 5, at the end of twelfth cycle). This descriptive and prospective study was conducted with 84 BC patients receiving paclitaxel regimen. This longitudinal study firstly aimed to investigate symptom status, body perception changes, and the risk of anxiety and depression in BC patients receiving during paclitaxel regimen. Paclitaxel regimen which is widely used in clinical treatment causes many negative physical and psychological consequences on women with breast cancer (BC).


 0 kommentar(er)
0 kommentar(er)
